Myopia (Dillon Brown)
Myopia, colloquially referred to as “nearsightedness”, is the most common cause of visual impairment worldwide that stems from a mismatch between optical power and eye geometry (refractive error). The incidence rate of myopia has been steadily increasing since the 1960’s in most populations (Figure 1), projected to affect nearly 50% of the world’s population by 2050 [1]. Not only is myopia a major economic burden globally, but it is also a risk factor for many other potentially blinding ocular conditions, including glaucoma, retinal detachment, and macular degeneration, regardless of a person’s use of optical correction methods (e.g. glasses). Taking this risk into account, myopia is estimated to be the second leading cause of blindness worldwide [2].
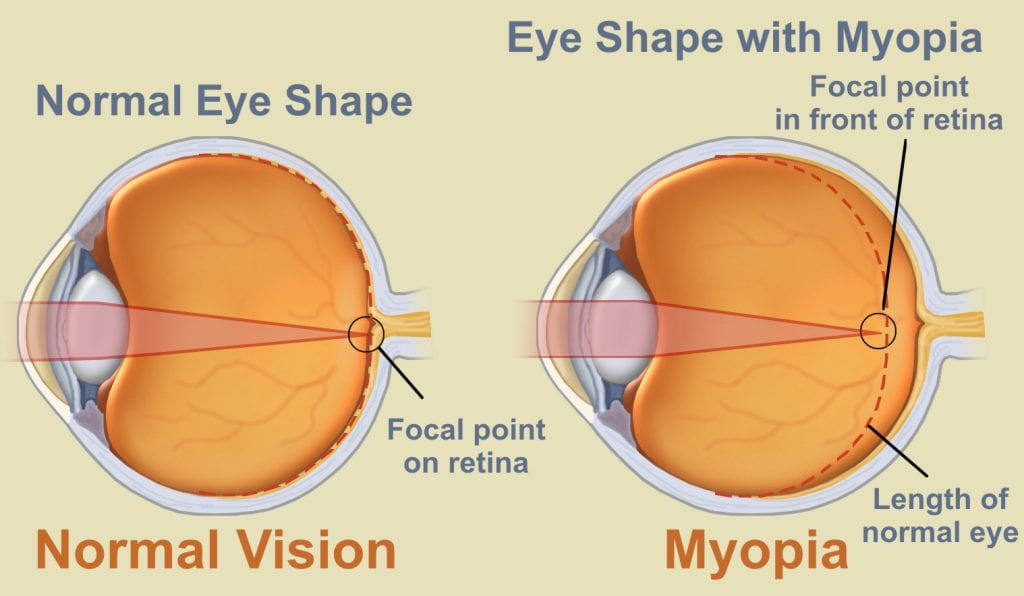
In 95% of myopia patients, excess elongation of the eye is responsible for the refractive error (Figure 2). While available optical correction techniques have improved dramatically, they universally fail to address this change in geometry responsible for the increased risk of other conditions.
Data suggest that 1) the sclera (connective tissue shell of the eye) is responsible for maintaining overall eye shape and size by resisting the expansive intraocular pressure (IOP) and 2) that scleral remodeling occurs with myopia in humans and all animal models investigated. Thus, microstructural remodeling of the sclera likely confers changes to tissue level mechanics that leads to a different deformation of the sclera under the IOP and thus an elongated eye; however, the exact relationship between these remains elusive.
Our Research:
The goal of our lab, in collaboration with the Pardue Lab, is to explore microstructural changes in the sclera and how they relate to tissue level mechanical properties in the mouse model of myopia. Ocular biomechanics research in the mouse model presents many challenges, but it enables us to utilize a wide array of genetic mutants to probe the myopia remodeling pathway. A deeper understanding of this pathway could lead to pharmacological therapies that target the underlying pathological changes that lead to changing tissue level biomechanics, resulting in a slowed/halted elongation of the eye.
We hypothesize that the proteoglycan aggrecan is a crucial molecule for proper scleral function, and early changes to aggrecan content observed in eyes developing myopia may change the biomechanical environment to stimulate further remodeling by the resident cells. Our lab is using compression testing and a poroelastic material model to extract scleral properties relating to permeability and tensile and compressive stiffness, novel in the mouse. These measures will likely be sensitive to aggrecan content and will enable a deeper understanding of the changing biomechanical environment.
[1] Holden, B.A., et al., Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology, 2016. 123(5): p. 1036-42.
[2] Fricke, T.R., et al., Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ, 2012. 90(10): p. 728-38.
[3] Wolf, N. (2016, April 07). How to stop myopia progression? Retrieved from http://www.precisionfamilyeyecare.com/how-to-stop-myopia-progression/